Improving Medicine Through AI – Sponsored by White Plains Hospital

Special promotional content provided by White Plains Hospital
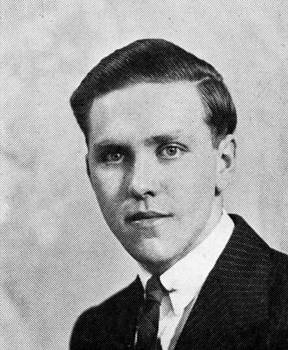
By Dr. Anthony Mercando, Cardiovascular Disease, Cardiology

The promise of Artificial Intelligence (AI) appears to be limitless in practically every area of life, including medicine. As White Plains Hospital’s newly named Coordinator of AI Projects, I am exploring its technological possibilities as well as maintaining my clinical practice in cardiology.
First and foremost, I view AI as a tool – not as something that is designed to replace physicians or nurses, but as something that can augment and improve their professional lives. One case in point is the FDA’s clearance earlier this month of Eko Health’s Low EF detection AI – something that can benefit and save time for both patients and physicians. The California company, which is funded in part by the Mayo Clinic, specializes in digital stethoscopes that use AI software to provide such features as noise-cancelling, high-fidelity audio (especially useful in an emergency room setting) and a 3-lead electrocardiogram (ECG), which can be used to detect cardiac disease.
This latest development will allow primary care physicians to detect low ejection fraction (EF), a measurement of how much blood the left ventricle pumps out with each contraction, within 15 seconds. An EF of 50-70% is considered “normal” for most patients, though it is still possible for a patient to experience heart failure if their EF is within that range.
Although I routinely use Eko stethoscopes, I have not had the chance to test this newest software. Even so, its value seems clear: if a PCP gets a reading below 50 – and the patient has other contributing factors, such as age, past history, genetic history and the like – it may be advisable to order an echocardiogram and take further measures, including a referral to a cardiologist.
Again, it is important to note that an unfavorable reading on the stethoscope does not in and of itself mean the patient is suffering from heart failure. As mentioned above, further steps need to be taken, preferably without panicking the patient.
Still, time can be of the essence. In the U.S., more than 6 million people suffer from heart failure, with half of them experiencing heart failure with reduced EF. Unfortunately, many heart failure cases go undiagnosed until symptoms force a visit to a specialist or ER.
As it currently stands, the Low EF AI is showing 74.7% sensitivity and 77.5% specificity – impressive numbers but obviously not at a fail-safe level. However, as time goes on and more data is collected, we can anticipate those percentages rising because of further tuning of the AI model.
With my assistance, White Plains Hospital is exploring numerous AI developments, including ambient dictation technology, which transcribes and summarizes conversations between physicians and patients to generate office notes, which should be a time-saving tool; streamlining how electronic patient data is reported and accessed; and answering questions that patients post in our portal in a more efficient manner.
I want to emphasize that I do not see AI as anything other than a tool, especially in medicine, where the human factor will always be an important part of any process.
That said, the future of this technology shows much promise in healthcare, and I look forward to learning (and potentially using) more.
Dr. Anthony Mercando is a board-certified cardiologist at White Plains Hospital Physician Associates. To make an appointment, call 914-849-4800.
Health Matters
The original version of this article was published in Health Matters, a White Plains Hospital publication.